KYPHOSIS
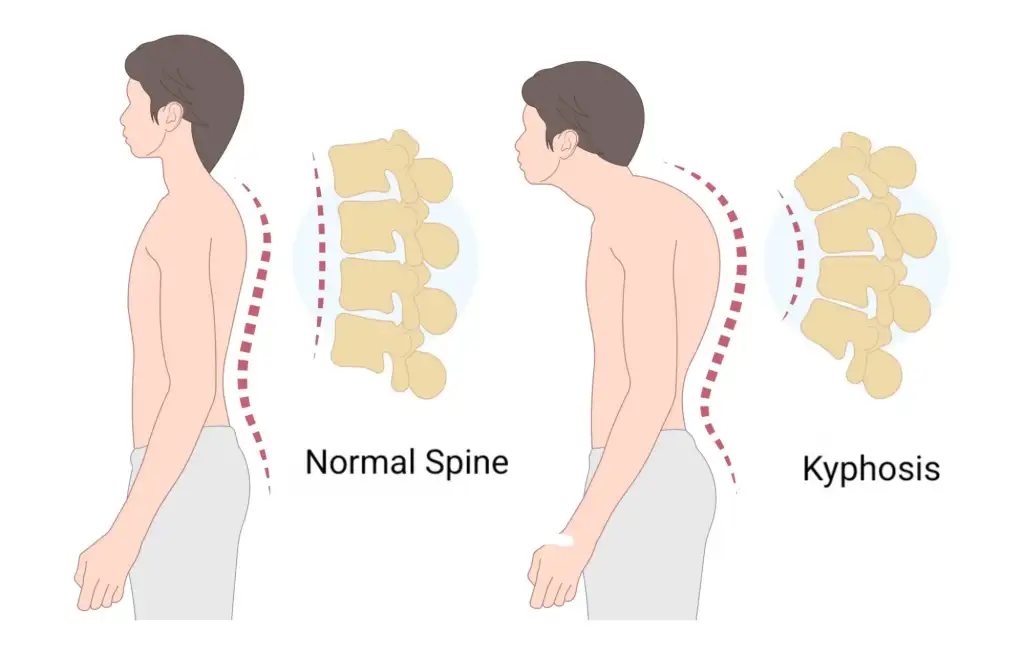
The human spine is not a straight line when viewed from the side. There is kyphosis (hunchback) in the thoracic and dorsal region and hollowness (lordosis) in the lumbar region. The kyphosis normally found in the thoracic and dorsal regions varies between people. Some people stand more hunched while others stand more upright. The physiologically accepted limit of this hunchback is between 20 and 55 degrees. The degree of hunchback can be determined on a lateral radiograph taken in a comfortable standing position. People with kyphosis suffer from widespread back pain. When viewed from the back, the normal spine appears straight along its entire length. From the side, there are three visible natural curvatures. There is a C-shaped curve in the neck called cervical lordosis, followed by a thoracic curve called thoracic kyphosis and a C-shaped curve in the lumbar region known as lumbar lordosis. These curves keep the head and torso balanced on the pelvis. These curves are interrelated and changes in one curve can affect the other curves. Increased curvature in the back is called “kyphosis”, “kyphotic deformity” or “hunchback”. In response to this, the curvature in the lumbar region may increase.
1. Postural kyphosis
It is the most common form of kyphosis and is related to posture disorder. The most important difference from other types of kyphosis is that kyphosis can improve when standing upright due to flexibility. Factors such as prolonged desk work, poor posture during the use of devices such as computers and tablets, and lack of sportive activity are facilitating factors. It can be corrected by correcting sitting habits, exercises that correct the spine, exercises that strengthen the abdominal, back and waist muscle groups and sportive activities such as swimming. However, if neglected, the posture disorder loses its flexibility over time.
2. Congenital kyphosis
3. Scheurmann Kyphosis
This deformity, also known as structural kyphosis, occurs as a result of wedging of the vertebrae during puberty. The exact cause of this phenomenon is unknown, but it is thought to be multifactorial and is more common in males. Hyperkyphosis (abnormal forward bending of the thoracic spine) can be divided into postural and structural. Postural kyphosis disappears when the patient stands straight. Patients with postural kyphosis have no spinal deformity. It is often seen between the ages of 12 and 15. Abnormal kyphosis is best detected when the patient is leaning forward. Patients with “Scheurmann’s disease” often present with posture disorder and back pain. Back pain is often present in early adolescence and decreases with age. The pain increases with daily activities. Kyphosis is often symptomatic and its apex is often located in the middle and lower part of the thoracic spine rather than the upper part.
4. Psotraumatic kyphosis
Posttraumatic kyphosis is often seen in the thoracolumbar and lumbar region after fractures. Patients with this type of kyphosis often have neurological damage such as paralysis. Kyphosis may be associated with chronic pain. Causes of pain include spinal muscle weakness, chronic inflammation, progressive deformation and compression of the spinal cord or nerve roots.
5. Postinfectious
The term “postinfectious kyphosis” refers to kyphosis, a specific condition caused by an infection. Kyphosis refers to a greater than normal forward curvature of the spine. Postinfectious kyphosis usually occurs after spinal damage caused by an infection.
6. Secondary to osteoporosis
Osteoporosis is a condition in which the density of bones decreases and bones become brittle. Osteoporosis can often develop due to factors such as aging, hormonal changes (especially menopause), low calcium intake and vitamin D deficiency.
1. Observation
It is often the first line of treatment in young children with spinal deformities. Significant changes are recorded each time patients come for examination by measuring the differences on direct radiographs. More than 45 degrees of severe or progressive congenital kyphosis deformity or kyphosis associated with neurologic weakness is often treated surgically. An early surgical approach usually gives the best results and stops the progression of the curve. Depending on the nature of the deformity, the surgical procedure varies. Observation is recommended in the following cases:
- Postural hyperkyphosis
- Curvatures less than 60 degrees in the growing age
- Curves of 60-80 degrees with incomplete growth spurt
Check-ups are done every 6 months with radiographs taken standing up on a long scoliosis tape. If the child has pain, an exercise program is often recommended.
2. Corset treatment
Corsetry is not recommended in the treatment of congenital kyphosis. Clinical studies are insufficient to evaluate the results of patients treated with this method. In developmental kyphosis, if the deformity is moderate (60-80) and the patient has not completed bony development, bracing may be recommended in conjunction with an exercise program. Full-time use of the brace (20 hours a day) is recommended until maximum improvement is achieved. In the last year during the completion of skeletal development, corset use may be reduced to 12-14 hours a day. Corset use should be continued for at least 18 months to achieve a complete and permanent improvement.
3. Surgical treatment
Treatment of kyphosis aims to correct and stabilize the deformity, reduce pain and improve neurological function. Flexible deformities can only be treated with posterior fusion and instrumentation (connecting the vertebrae with screws and rods). Depending on the degree and stiffness of the kyphosis, osteotomy (bone removal) may also be recommended. The so-called “Ponte osteotomy”, which involves the partial removal of only the posterior elements of the spine, or the “Pedicle subtraction osteotomy”, which involves the removal of a wedge-shaped portion of the spine, may be required. For more advanced and severe curvatures, a vertebral resection osteotomy may be performed to remove the anterior and posterior elements of the spine from the posterior (back) region. Our clinic is one of the most common centers in the world to perform this technique, called posterior vertebral column resection (PVCR). It may also be necessary to perform several of these procedures together. These osteotomy procedures, which are highly specialized and require a certain level of experience, have been performed in our department for many years. With the increase in experience, special osteotomy techniques developed in our clinic and presented and accepted in various scientific platforms are also applied in appropriate patients. Fixed deformities often require more serious surgeries involving removal or amputation of the vertebrae. All these procedures are successfully performed by the experienced surgeons of our clinic. Postoperative corset use is the same until union is detected on control direct radiography. Patients can return to their normal daily activities within 4-6 months. The change provided by surgical correction is visible.
In situ fusion:
The surgical choice for progressive kyphotic deformity is complete fusion or arthrodesis (fusion of the vertebrae) of the deformed spine. Fusion should include the upper normal spine and the lower normal spine. Bone graft from the patient or from a tissue bank is used, placed posteriorly (dorsally). In severe angulated curves, an additional bone graft can also be placed anteriorly. With bone grafts, 4-6 weeks are needed until complete union tissue is formed. During this period, the patient should be supported with a cast or corset until complete union occurs.
Instrumented fusion and osteotomy:
Progressive kyphotic curves in older children may require instrumentation (rods, hooks and screws). If the spinal cord cannot tolerate techniques to lengthen the spine, the surgeon may consider removing the vertebra causing the deformity. The postoperative period of wearing a brace or cast is the same until union is detected on direct radiography.
Spinal fusion:
Surgical treatment may be recommended if the kyphotic deformity is severe (more than 75 degrees) and the patient has increased back pain. Surgical treatment provides significant improvement and there is no need to use a corset after surgery. Screws are inserted into the vertebrae and fixed with rods to straighten and lengthen the spine. Surgeries are often performed through back surgical interventions. Patients can return to their normal daily activities within 4-6 weeks. The change provided by surgical correction is immediately visible after surgery.
